What Type of Asthma Do You Have?
It's possible to have more than one
ByPat Bass, MD Pat Bass, MDDr. Bass is a board-certified internist, pediatrician, and a Fellow of the American Academy of Pediatrics and the American College of Physicians.Learn about our editorial processUpdated on February 15, 2022Medically reviewedVerywell Health articles are reviewed by board-certified physicians and healthcare professionals. Medical Reviewers confirm the content is thorough and accurate, reflecting the latest evidence-based research. Content is reviewed before publication and upon substantial updates. Learn more.byDaniel More, MD Medically reviewed byDaniel More, MDDaniel More, MD, is a board-certified allergist and clinical immunologist. He is an assistant clinical professor at the University of California, San Francisco School of Medicine and currently practices at Central Coast Allergy and Asthma in Salinas, California.
Learn about our Medical Review BoardTable of ContentsView AllTable of ContentsThere are several types of asthma. They all have similarities, but some have unique aspects that affect how they're triggered, diagnosed, and treated.
Common asthma types include:
Exercise-induced bronchoconstriction is often included in this list as well, though not everyone who experiences it actually has asthma.
This article explores the most common types of asthma, what additional symptoms they cause, and what extra diagnostic tests and treatments they require.
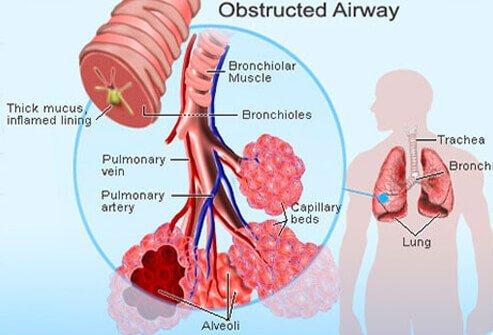
What Asthma Types Have In Common
Asthma has certain features that remain the same across most types:
Because of this, it's easy to assume that all types of asthma are fundamentally the same. While that's true to a certain extent, the differences between the types matter. That makes an accurate diagnosis crucial.
Determining Your Asthma SeverityAllergic Asthma
Allergies are involved in between 50% and 80% of asthma cases. People with seasonal allergies (hay fever) may also be diagnosed with seasonal allergic asthma.
Common triggers of allergic asthma include:
Classic asthma symptoms are accompanied by allergy symptoms, such as:
Allergic asthma is believed to have a heavy genetic component plus hypersensitivity and exposure to the triggering substances.
To confirm allergic asthma and determine your triggers, your healthcare provider may also order:
You'll need to manage both asthma and allergies. That may include avoiding triggers, taking allergy medicine (antihistamines), or allergy shots (immunotherapy).
All About Allergic AsthmaAllergic asthma is the most common type. It may be triggered by pollen, mold, and other allergens. It's likely caused in part by genetics. Skin and blood tests can diagnose it. Treatments include avoiding triggers, antihistamines, and immunotherapy.
Non-Allergic Asthma
Between 10% and 33% of all people with asthma have non-allergic asthma. It usually develops later in life than allergic asthma.
Some research suggests non-allergic asthma is more severe than other forms. Some studies also suggest it's more common in women.
Non-allergic asthma symptoms can have a variety of triggers, including:
Non-allergic asthma isn't associated with additional symptoms.
Things that may lead to non-allergic asthma include:
Conditions such as rhinosinusitis (inflammation of the nasal and sinus cavities) and gastroesophageal reflux disease (GERD) frequently affect people who have non-allergic asthma and may contribute to its development.
No test can specifically diagnose non-allergic asthma. Diagnosis can involve skin and blood tests to rule out allergies.
You may not need treatments beyond what's generally prescribed for asthma.
However, some people with non-allergic asthma don't respond well to inhaled corticosteroids (ICS). These drugs are used as daily preventive medication for moderate-to-severe asthma.
If ICS don't work for you, you may need other preventive drugs such as:
Non-allergic asthma is triggered by irritants. It often comes on later than allergic asthma and may be more severe. Second-hand smoke, viruses, or certain medical conditions can trigger it. Diagnosis involves ruling out allergies.
Cough-Variant Asthma
A dry cough is the main symptom of cough variant asthma (CVA). It may remain your sole symptom. Or you may go on to develop other symptoms, especially if it's not adequately treated.
Because a dry cough doesn't usually make people think they have asthma, symptom triggers are an important part of figuring out you have the condition.
Watch for bouts of coughing that:
CVA doesn't have additional symptoms.
Cough-variant asthma may be an early symptom of emerging asthma; children have it more often than adults. Even so, only about 30% of people with CVA develop classic asthma.
CVA is hard to diagnose. In addition to standard asthma tests, your healthcare provider may order a sputum test to look for white blood cells that are often increased with asthma. Sputum is a type of mucus that's coughed up from the lungs.
Treatment for cough-variant asthma is generally the same as for other types of asthma.
Could Your Dry Cough Be Asthma?Cough-variant asthma's only symptom may be a dry cough. That makes it harder to recognize. It's tied to exercise, cold and dry weather, and hay fever or other allergies. In some, it may be an early sign of developing asthma. It's diagnosed with a sputum test.
Get our printable guide for your next doctor's appointment to help you ask the right questions.
Download PDFEmail the GuideSend to yourself or a loved one.
This Doctor Discussion Guide has been sent to {{form.email}}.
There was an error. Please try again.
Nocturnal Asthma
Nocturnal asthma, as a diagnosis, is usually added to a pre-existing asthma diagnosis. If you have marked nighttime symptoms, you might have nocturnal asthma or it could be that your asthma is not well controlled.
More than 50% of adults with asthma have nocturnal asthma. About 10% of children with asthma have this form as well.
With nocturnal asthma, you may experience nighttime symptoms several times a week or even every night.
Environmental symptom triggers can include irritants like pet dander or dust in your bedroom or sleeping with the window open.
The symptoms of nocturnal asthma are the same as classic asthma symptoms. They just happen to be more prominent at night.
Sleep interruptions from nocturnal asthma can leave you tired during the day. You may notice you're waking up several times overnight. But many people fall back to sleep quickly and don't recall waking up.
Nocturnal asthma can increase your risk of serious complications, including heart disease, respiratory arrest, and asthma-associated death.
Nocturnal asthma is believed to be caused by changes in your body that occur at night.
Your circadian rhythm, which is your internal body clock, contributes to nocturnal asthma by causing nighttime shifts in:
Additionally, obstructive sleep apnea, a sleep disorder that interrupts breathing during sleep, is common among people who have asthma. And the conditions can exacerbate one another.
Testing your breathing during the day isn't helpful in diagnosing nocturnal asthma. So, your healthcare provider may have you test your breathing with an at-home monitor close to your bedtime.
Depending on your symptoms, you might also be sent for a sleep study. For that, you spend the night at a sleep lab and have your symptoms monitored. Some sleep studies can also be done at home with special equipment.
Nocturnal asthma is treated with the same medications as classic asthma. But it may require adjusted timing of your medication.
For example, rather than taking a daily control medication in the morning, you might take it in the afternoon or early evening.
Some researchers have suggested time-release tablets for treating this type of asthma. These dissolve slowly so they're effective over a longer period of time.
Managing Nocturnal AsthmaNocturnal asthma strikes several nights a week. Triggers are irritants in the air. It has a higher risk of asthma-related death. You may need to test your breathing close to bedtime for a diagnosis. Daily control medication may be taken in the afternoon or evening instead of the morning.
Exercise-Induced Bronchoconstriction
Exercise-induced bronchoconstriction (EIB) used to be called exercise-induced asthma (EIA).
Up to 90% of people with any type of asthma may have exercise-related symptoms. However, many people with EIB don't fulfill the diagnostic criteria for asthma.
In EIB, your bronchial tubes (airways) narrow when you exercise. It's believed rapid breathing during exercise can dehydrate the bronchial tubes, which then constrict.
Typically, symptoms begin during exercise but may continue getting worse for 10 to 15 minutes after you stop.
They generally clear up on their own within 30 minutes. But it's safer to use your rescue inhaler than wait to see if you improve without it.
When combined with exercise, certain factors may make EIB more likely. They include:
Low-intensity activities (walking, hiking) or sports with short bursts of exertion (baseball, wrestling, gymnastics) are less likely to trigger EIB.
EIB can have a few symptoms not common in asthma, including:
If you have asthma, minor irritation or dehydration from exercise may cause EIB. In this case, the cause of EIB is underlying asthma.
For people who don't have asthma, repeated exposure to cold, dry air or airborne irritants while exercising may damage bronchial tubes and cause EIB.
This may explain why EIB is especially common in cold-related sports (ice hockey, skiing) and among competitive swimmers (due to chlorine fumes).
People with environmental allergies, or who have close relatives with environmental allergies, have a higher risk of developing EIB.
Whether or not you've been diagnosed with asthma, your healthcare provider may test your breathing before and after exercise to determine whether you have EIB.
They'll check your forced expiratory volume (FEV1), which is a measure of how much air you can force out of your lungs.
Then you'll exercise while being supervised, and your FEV1 will be measured again. A decrease of 15% or more generally leads to a diagnosis of EIB.
If you're also diagnosed with asthma, preventing bronchoconstriction will be part of your overall treatment plan.
You may be able to prevent symptoms of EIB by:
Your healthcare provider may recommend:
Understanding EIBExercise-induced bronchoconstriction is triggered when exercise causes dryness in the airways. It's worse in the cold, in hot air, and around chlorine fumes. FEV1 tests before and after exercise are used for diagnosis. Using an inhaler before exercise may prevent attacks.
Occupational Asthma
Some jobs expose you to substances that can lead to occupational asthma (OA). This may account for about 15% of asthma cases in the U.S.
If you have other forms of asthma, these same workplace exposures can make your symptoms worse.
More than 250 substances are believed to cause and trigger OA symptoms. Typically, symptoms are only triggered by the substance(s) you're in regular contact with.
Common triggers include:
Many other potential triggers exist, as well.
Many people with IgE-mediated (allergic) asthma develop occupational rhinitis (nasal allergy) symptoms prior to the onset of OA symptoms.
Symptoms from work-related exposures can happen right away or take years to develop.
Regular exposure to fumes, gasses, dust, or other irritants causes OA. The exposure either directly damages your airways or causes sensitization to the offending substance.
With sensitization, your body gradually develops an abnormal immune reaction to a substance. You're at risk for OA if you work in/at a:
This list is far from complete. Many other workplaces may expose you to potentially problematic substances.
If you outgrew childhood asthma or have a family history of asthma, you're more likely to develop the occupational type.
Employers are required to provide Material Safety Data Sheets (MSDS) for any hazardous substances you may come into contact with at work. Having these can help your healthcare provider identify substances that may be triggering your asthma.
If your provider determines you have asthma and rules out seasonal allergies as a trigger, they can start investigating work-related causes. It can help if you provide Material Safety Data Sheets for chemicals you're exposed to at work.
The next steps can include:
Occupational asthma is sometimes misdiagnosed as bronchitis. If you're diagnosed with bronchitis but treatment isn't effective and symptoms tend to be worse at work than in other places, bring this up with your healthcare provider.
Getting a proper diagnosis and treatment is important. If OA continues unchecked, it can cause permanent lung damage.
Standard asthma treatments are typically used for OA. In addition, you'll want to take steps to avoid the problem substance(s) if possible.
This may require Reasonable Accommodation from your employer, which is required under the Americans With Disabilities Act (ADA). Some people have to change jobs to avoid their triggers.
How Irritants Cause AsthmaOn-the-job exposure to chemicals or other irritants can lead to occupational asthma. Common triggers include animals, flour, mold, and cleaning products. Diagnosis can be difficult. Avoiding triggers is important. This may require Reasonable Accommodation or changing jobs.
Other Types of Asthma
Asthma comes in several less-common types, as well.
Obese asthma is a recently identified asthma type. It appears to be different from other types of asthma, even in people with obesity. Genetics studies suggest airway constriction comes from a different mechanism.
Obese asthma is a stand-alone diagnosis. Research suggests it has a different genetic and molecular basis plus many other unique characteristics. Not everyone who's obese and has asthma has obese asthma.
Medication-induced asthma is triggered by aspirin and a few other medications. It's believed to have a genetic susceptibility.
This can be a stand-alone diagnosis or it may be added to a previous asthma diagnosis. It typically makes pre-existing asthma worse. It can be severe and even fatal.
In viral-induced asthma, a respiratory tract infection (e.g., the common cold, flu, or COVID-19) can trigger or worsen asthma. An estimated 50% of acute asthma attacks have a viral trigger.
This type can also be a stand-alone or add-on diagnosis.
Glucocorticoid-resistant asthma is a subtype of asthma. It's defined by symptoms that don't respond to the steroid treatments frequently used for asthma. It's especially likely to be severe.
Glucocorticoid-resistant asthma is always an add-on to an earlier asthma diagnosis.
Some researchers say that "asthma," as a global term, could become obsolete in favor of terms that better describe the mechanisms associated with the various types.
Naming Your Asthma
It's not uncommon for asthma to be called by several different names.
It may be referred to by its:
Classifying Asthma by SeverityAnd as discussed, some of these classifications may also be combined—for example, mild intermittent adult-onset allergic asthma, or glucocorticoid-resistant occupational asthma.
It's also possible to have more than one type of asthma. For example, you could have non-allergic and nocturnal asthma.
If you're unsure what's behind the name being used to describe your case, be sure to ask your healthcare provider.
These are more than just names. They indicate something about your condition that is important to its management, among other things.
For example, compared to childhood-onset asthma, adult-onset asthma typically:
Summary
Asthma comes in many forms and can develop at any age. Allergic asthma is triggered by allergies. Non-allergic asthma is triggered by irritants in the air.
Cough-variant asthma is distinguished by a dry cough. Nocturnal asthma is worse at night.
Exercise-induced bronchoconstriction isn't true asthma but is common in people with asthma. Occupational asthma is triggered by workplace exposure to irritants.
Less common types are triggered by certain medications or viruses. One type involves resistance to standard asthma treatments.
Some types have to be diagnosed and treated differently from classic asthma.
A Word From Verywell
Zeroing in on an accurate asthma diagnosis can take some time. Your precise diagnosis can have a big impact on the treatments you're given, so the diagnostic process is important.
Pay close attention to your symptoms, their frequency, triggers, and factors that may have influenced the onset to help your healthcare provider reach the correct diagnosis and treatment plan for you.
Viral-Induced Asthma and How to Treat ItWas this page helpful?Thanks for your feedback!Sign up for our Health Tip of the Day newsletter, and receive daily tips that will help you live your healthiest life.
You're in!Thank you, {{form.email}}, for signing up.
There was an error. Please try again.
What are your concerns?26 SourcesVerywell Health uses only high-quality sources, including peer-reviewed studies, to support the facts within our articles. Read our editorial process to learn more about how we fact-check and keep our content accurate, reliable, and trustworthy.Additional Reading